What is fertility preservation (FP)?
Fertility preservation measures are usually taken when a patient has to undergo certain fertility- altering treatments/procedures or is at risk of losing his/her fertility early before completing their family. FP can help patient shift focus to getting better, reduce uncertainty and remain hopeful without worrying about not being able to have children later.
Most common reasons for opting for FP are when one of the partners is in a high-risk job like the military or there is family history of pre-mature ovarian failure/ infertility. FP is most widely employed for a person diagnosed with cancer that could affect fertility. This article is mainly focussed on fertility preservation for cancer patients – Oncofertility.
The diagnosis of cancer can be a life-altering event. The stress increases many-fold if the patient wants to have babies in the future as certain cancers or its therapies can have debilitating effects on fertility.
A new field, “Oncofertility”, has emerged which is an amalgam of reproductive medicine and oncology. Oncofertility experts guide patients in preserving their fertility and strive for them to experience the joys of parenthood by aiding in conception after cancer treatment.
This field involves collaborative expertise of oncology, fertility, endocrinology specialists.
How does cancer/ treatment cause infertility?
Depending on the cancer, target organ or method of treatment, there can be damage to the reproductive organs leading to poor quality of gametes, lowered sperm count, DNA damage to eggs and sperms, premature menopause and subsequently infertility.
Surgery: In some kind of cancers, the entire affected organ might need to be removed (especially in ovarian, uterine cancers). Sometimes just the tumor might be removed which may cause scarring or blockages leading to difficulty in ovulation or sperm delivery. Getting pregnant or carrying a pregnancy might become difficult in such conditions.
Chemotherapy: Certain drugs are used to target fast dividing cancerous tumor cells to stop their spread. The side-effects is that they can attack normal fast-diving cells of the body as well. Depending on the dose and duration of chemotherapy, there can be various effects on fertility:
- woman’s eggs might get damaged – DNA damage and poorer quality leading to difficulty in conceiving, higher pregnancy loss and/or birth defects rates
- Irregular periods and early menopause
- Sperm cells are fast-dividing cells and chemotherapy directly damaging sperm cells or causes hormonal imbalance, impairing sperm production
Radiation/ Radiotherapy: Specific type of rays are used to target the tumor cells’ DNA to slowly kill the cancer cells. These rays however also affect the tissues and organs surrounding the target organ. Thus radiation used in pelvic or abdominal part or around the brain can damage the reproductive organs by scarring or damaging their DNA or fertility hormone production.
Effects of radiation may be long-term (untimely menopause or no sperm production after a few years) or temporary (reduction in fertility for a while around treatment).
Fertility preservation techniques:
Oncofertility interventions are ideally to be done before starting cancer therapy while being mindful of the patient’s condition. These need to be timed well depending on the urgency to start cancer treatment under the guidance of the treating oncologist, fertility expert, endocrinologist.
- Egg cryopreservation (freezing): Patient’s ovaries are stimulated using medication and hormonal injections to produce higher number of eggs. These eggs once released, are retrieved by a simple procedure called ovum pick-up and are carefully frozen and stored in liquid nitrogen to keep them viable for future use. This process may take about 15 days to a month depending on the time of the cycle the patient is at.
- Sperm cryopreservation: Men can provide the semen sample which is tested for sperm count and quality and frozen in liquid nitrogen to keep viable for years without any damage.Sperms can be obtained by testicular sperm extraction/aspiration (TESE/A) for men who cannot provide semen sample/ semen does not contain sperms/ sperms of poor quality. This involves getting sperms directly from the testes via a minor surgery (testicular biopsy).
- Embryo cryopreservation: This is a more effective FP option especially for female patients having partners. The eggs are retrieved as with egg freezing, sperms from the male partner are taken and fertilised via IVF or ICSI. Embryo(s) is grown for 5 days under specific conditions and carefully stored at very low temperatures in liquid nitrogen. These can be used once the woman is cancer-free or in a surrogate. The success rates of fresh and frozen embryos are similar and fairly high. This process might also take about 3 to 6 weeks.
Since both egg and embryo freezing involve using hormones, patients with certain types of hormone- sensitive cancers may not be able to avail these. There may be tweaks in the egg stimulation protocol depending on type of tumor.
Both these techniques also require some time before cancer treatment can be started. Thus these may not be useful for women who need to be treated urgently.
Thus, it is essential to check for the type of cancer/tumor before deciding on the FP technique.
- Shielding: Radiation in the abdomen or pelvic area can also spread to reproductive organs. Shields (usually made of lead) are used to protect the healthy surrounding organs from the radiation. These are placed around the testes and lower abdomen/pelvis for women, through which the rays cannot penetrate and cause damage. This method not effective for chemotherapy and also if the target organs for radiotherapy itself are the testis/ovaries.
- Ovarian Transposition: This method too is used for protection against side-effects of radiation. The ovaries are surgically moved into the abdomen, away from pelvis when it is the radiation target. The ovaries can be moved back into their original place once cancer treatment is complete. This however is not a fool-proof FP method as ovaries might fall back into the pelvis or radiation may still reach the ovaries in the abdomen.
- Trachelectomy/Cervicectomy: This is used in cases of early diagnosed cervical cancer cases. It involves removal of only the cervix, part of the vagina and surrounding tissue, while sparing the uterus, thus giving women a chance to conceive later.
- Ovarian Suppression: This is a relatively recent technique. Certain medications are used to reduce the ovarian function causing a temporary menopause-like state to protect the egg quality from ill-effects of chemotherapy. Post cancer treatment, ovarian function is restored.
- Ovarian tissue freezing and transplant: This is still an experimental technique especially useful for girls who have not started menstruating to protect their immature egg follicles or for women whose chemo/radiotherapy cannot be postponed till egg retrieval.It involves removal of some part of the ovarian tissue (cortical tissue containing the egg follicles) via laparoscopic surgery before starting cancer therapy and frozen. Post onco-treatment, the tissue is transplanted back to restore normal ovarian function (hormone release and ovulation), which may happen within a few months. Though experimental, many live births have been reported using this technique.
Post cancer:
Post cancer treatment, the patient’s fertility needs to be assessed by a fertility specialist. Trying for a baby should start under the treating oncologist and fertility expert’s guidance.
Patients who have been unable to get fertility preservation prior to cancer treatment and have lost their fertility potential can still get pregnant through other means:
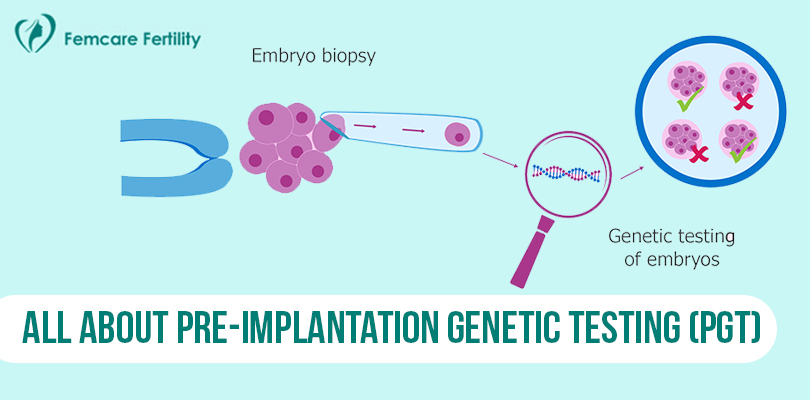
- IVF (with or without PGD) can be used for women who still have some fertility potential post treatment.
- Gamete donors – Egg or sperm donors can be used for IVF
- Surrogacy – For women who cannot carry pregnancies post treatment (but may have their eggs stored) or women who are at higher cancer recurrence risk if pregnant
- Adoption
Future of oncofertility:
Oncofertility measures in patients have proven to be quite effective. Thus this field, though fairly new, is a rapidly advancing one with a promising future for couples in need. Oocyte maturation outside the body (in-vitro), testicular tissue freezing and transplantation, use of spermatogonial stem cells are techniques particularly helpful for pre-adolescent children suffering from cancer and at-risk of losing fertility. These techniques have shown promise in the labs to be used in the future.
As the best infertility clinic in Pune, we at Femcare Fertility understand the turmoil a couple goes through in conditions where they may lose their fertility early, especially with a life-changing diagnosis. The best fertility doctor in Pune provides rapid, actionable solutions with utmost sensitivity, for the couple to make an informed choice. We strive to support the patient and couple throughout their pre and post cancer journey of fertility preservation.