The ultimate, but rather impossible, dream that we harbour is to remain youthful forever and stop our bodies from ageing!
The idea of being able to suspend our cells in time seems straight out of a sci-fi movie. While we may not be able to prevent our bodies from growing old, different means need to be discovered and utilised to preserve fertility as rising age of having babies, lifestyle and stress have increased incidence of infertility globally.
With technological advancement, we have now achieved the feat of halting aging of gametes to keep them young and fresh for prolonged periods of time.
The word cryopreservation comes from the Greek word cryo meaning to freeze + preservation. This technique is popular in the medical field and its uses have been extrapolated to the fertility setting.
It involves preserving gametes or embryos at freezing temperatures to thwart all biological processes, reactions and activities in the cells in their present state without damaging them. When retrieved to be used again, the processes restart from where they had stopped, even after years.
History of cryopreservation in fertility:
Cryopreservation was first conceptualised for religious purposes to store the multiple, unused embryos from an IVF cycle which would be discarded.
However, sperms were the first specimen to be cryopreserved in the 1950s and there has been no looking back.
Around the same time, certain chemicals which could protect against formation of ice crystals on freezing were discovered. These cryoprotectants or cryopreserving agents, proved to be game changers as ice crystals are known to damage the insides of the cell as well as the cell membrane when thawed. These help to reduce physical damage to the cells caused by the crystals.
Eggs were the last to be frozen and preserved. A successful pregnancy and livebirth from a cryopreserved egg was in 1986. However, egg freezing was regarded as an experimental technique until a decade ago!
With technological sophistication, significant improvements have been made in this area, in terms of safety and successful outcomes.
Cryopreservation techniques:
The preferred medium for preservation is liquid nitrogen at a temperature of -196 °C or -321 °F, as it is non-reactive and non-toxic.
Two common cryopreservation techniques are:
1. Slow freezing:
It was the first cryopreservation technique, developed in the 1980s. The specimen (sperms/eggs/ embryos) is sealed in a tube with cryoprotective agents → Placed in a machine that gradually reduces the temperature inside over 2-3 hours → These vials are stored in liquid nitrogen tanks.
This technique is almost obsolete now, since there is a higher risk of ice crystal formation with longer freezing time.
2. Vitrification:
After being introduced in the mid-2000s, this technique has now become a preferred one for freezing cells. It works on the opposite principle of slow freezing. Cryopreservation agents are put in the specimen to reduce some amount of water from the cells → The specimen is then flash frozen by directly exposing it to liquid nitrogen at -196 °C and stored.
This almost eliminates the risk of icicle formation and cell damage, thereby improving viability.
Eggs frozen by vitrification better survived the freeze-thaw cycle (>90%) than slow frozen eggs (60%).
The Process:-
- For Eggs: The process starts in the same way as in IVF. The woman’s ovaries are stimulated using certain hormonal injections for about 2 weeks, for maturation of multiple egg follicles instead of just one. Once the follicles are matured, the eggs are retrieved from the ovaries using a thin needle passing from the vagina, under anaesthesia. The quality of the collected eggs is assessed, good quality eggs are frozen and preserved for future use.
The ideal age for oocyte preservation would be late 20s or early 30s, which is a fertile period to retrieve enough (at least 10 or more) good quality eggs.
- For Sperms: Sperms can be obtained from the semen collected by masturbation or through surgical means (testicular biopsy/ epididymal aspiration). Sperm quality is checked (number, motility, abnormal forms) and good quality sperms are stored in open or closed vials in liquid nitrogen, in what is popularly known as sperm bank. Sperms obtained surgically are frozen in suspension in specific media. Men providing samples via masturbation are instructed to refrain from ejaculation 3-5 days prior.
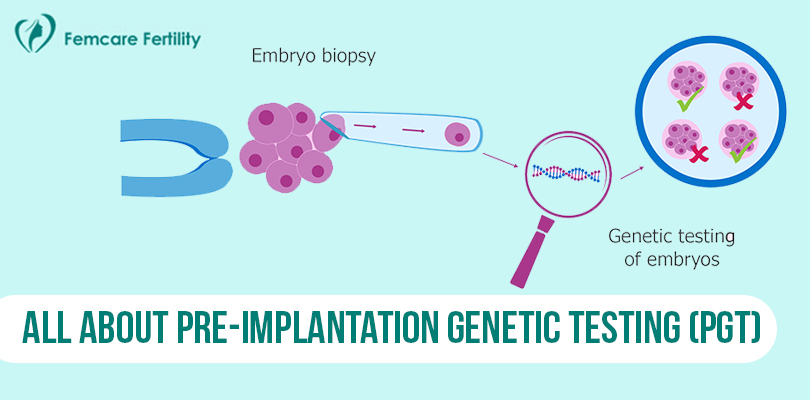
- For embryos: The option of preserving the unused embryos from an IVF cycle is offered as part of the IVF package or as an added service. Quality of the embryos is accessed before freezing and only best quality ones are frozen. Usually Day 5 embryos or blastocysts are stored.
Freezing sperms and embryos is easier than eggs as their high water content makes them susceptible to ice crystal formation and risk of damage on thawing. Sperms are hardier to cryopreserve due to lower water content.
Using the frozen cells:
For eggs or embryos: The cells are removed from the liquid nitrogen tanks → placed in a waterbath where temperature changes are gradually made → Cells are rehydrated and cryopreservatives removed.
Frozen eggs may need to be cultured before using.
Once thawed, eggs may be fertilized either by regular IVF (using fresh or frozen sperm) or by intra- cytoplasmic sperm injection (ICSI) where single, selected sperm is directly inserted into the egg for fertilization.
The embryo is allowed to grow and transferred into the intended mother’s uterus at the appropriate
time.
Frozen embryos can be put into the woman’s womb by a process called “Frozen Embryo Transfer”. This can be done either by use of medicines and hormones to stimulate thickening of the uterine lining or transfer is planned in tune with the woman’s natural menstrual cycle on a specific day.
Sperms can be thawed in a temperature-controlled warmer or at room temperature for 10 to 15 minutes. The quality of the sample is checked again, and viable ones are concentrated to be used for further processes (IUI/ IVF/ ICSI).
Why undergo cryopreservation ?
For eggs:
- “Social freezing” - To free women from the ticking biological clock and risks of infertility & abnormalities with increasing age. This gives women the freedom and autonomy to pursue their goals at their own pace before bringing a child into this world.
- “Fertility preservation” - Women diagnosed with cancer who may need chemo/radiotherapy which may damage their ovaries, fertility or in cases where removal of ovaries is essential for treatment.
- For women who are at risk of premature ovarian failure or have family history of pre-mature menopause
- In situations where sperms not available at the time of oocyte retrieval
For sperms:
- Fertility preservation for cancer treatment
- If sperms are retrieved via testicular biopsy (TESE) or aspiration from the epididymis (MESA/PESA) to avoid multiple invasive procedures
- Planned vasectomy
- For men working in high-risk jobs or their occupation involves exposure to substances which could hamper spermatogenesis
For embryos:
- In conditions where the intended mother’s endometrium has not thickened enough to transfer
- the embyo(s)
- To reduce risk of delayed ovarian hyperstimulation or wait for the ovarian environment and hyperstimulation to settle before transfer
- Store for future pregnancy planning to avoid undergoing the entire ovulation induction and ovum pickup process again
- To wait for results of pre-implantation genetic diagnosis to identify a healthy embryo devoid of genetic problems before transfer
Success:
Not every preserved sperm/egg/embryo can result in a viable pregnancy. However, over the years the success rates from frozen samples has steadily improved.
90-95% of the frozen eggs can survive the freeze-thaw cycle and are viable. Pregnancy success rates depend on the age of oocyte storage - for eggs frozen <35 years, success of fertilization is 70-80%, 20- 40% for implantation, 40-60% for successful pregnancy.
More than 5000 babies have been born using frozen eggs.
Some studies have concluded that the IVF success rate is moderately higher with frozen embryos (~8- 10% more) as compared to fresh ones.
In 2020, the world witnessed a record-breaking feat wherein a baby was born from an embryo frozen in 1992 !
Risks:
The freeze-thawing cycle and ice formation may damage some of the cells if not preserved and handled correctly. Eggs are more susceptible to such damage.
There is a small risk of hardening of the other layer of the egg cell/ embryo (zona pellucida), which may hamper penetration of sperm and/or implantation.
The risks associated with ovulation induction and egg retrieval remain as with IVF.
No increased risks to the future babies born from frozen cells in terms of birth defects or intellectual disability are known.
The future:
With ever expanding research in fertility medicine, newer techniques are being developed to freeze and save some ovarian tissue which can be transplanted back to restore fertility. Similar experiments are being tried on testicular tissues too.
Femcare Fertility is the best infertility clinic in Pune as we provide the latest, safest and most personalised fertility solutions. Our fertility specialist will guide you through the process of cryopreservation, when indicated and your samples will be stored in the prime of their health at one of the best cryopreservation setups in Pune.